Post-COVID Nursing
Post COVID nursing looks at what nurses had to face in the eye of the pandemic, what we have learned, and what may change for nurses. The year 2020 marked the 200th anniversary of the birth of Florence Nightingale, known for her profession-changing contributions to the field of nursing. The World Health Assembly dubbed 2020 the International Year of the Nurse long before they, or anyone else, knew what was about to come for nurses and others in the healthcare field.
Nurses – the Most Adaptable Healthcare Workers
Nursing has always been heralded as a difficult, exhausting, and often misunderstood profession. Many people have the idea that nurses go from patient to patient, providing comfort, when in reality a nurse’s job is far more scientific. 2020 and 2021 have proven that nurses continually rise above what’s expected, provide comfort and top-notch care to patients in need, and care in a way that’s often reserved for family and friends.
Throughout the pandemic, nurses have been faced with a system completely unprepared to take on a worldwide health disaster, and yet, they have risen above time and again. While nurses have stood up to the challenges of the pandemic, 2020 and 2021 have also led many nurses to think about how things need to change in order for the healthcare industry to be better prepared when the unthinkable occurs.
Need for New Technology
Nurses On the Front Lines
While the vast majority of the world was encouraged to stay home in an attempt to flatten the continually-increasing curve of the virus, nurses went to work, day in and day out, often staying in healthcare facilities for days at a time. Many nurses were forced to work with only makeshift personal protective equipment (PPE), including masks fashioned out of cloth that did little to protect them from contracting COVID-19, even while working with patients who had yet to be tested for the virus. Some nurses weren’t even able to get their hands on new cloth in the toughest times of COVID-19 and had to resort to using socks, garbage bags, and other materials that they were able to find lying around the hospital.
In addition to fear of contracting the virus, nurses and other healthcare providers also had to worry about taking the virus home to their families. Nurses shared stories of getting changed in the garage, being unable to go near family members until they showered after work, and simply sleeping at work rather than potentially exposing their family to the virus unnecessarily.
While the hard-working spirit of the nursing community was a wildly bright light in the midst of a terribly dark time, it’s clear that much needs to change in healthcare in order for nurses to get the treatment that they deserve. It’s also clear that the public at large needs to continue to appreciate nurses, rather than simply showing them a few months of appreciation during their darkest hours.
Now that nurses are able to get vaccinated and consider their future with less fear, we’ll take a look at how COVID-19 has changed the future of nursing, and what those who are thinking about applying for nursing jobs post COVID can expect. We’ll also explore how nursing school may change in order to better prepare future nurses in the event that something like COVID-19 happens again.
Growing Frustrated: What Nurses Have Had to Face During COVID-19
Nurses make up more than half of the healthcare workforce across the world. Patients, doctors, and other medical professionals rely heavily on nurses to ensure that patients get top-notch care and that hospital operations run smoothly. While most nurses know that their career is going to be stressful at times, few ever expected that they’d serve patients during a pandemic.
Even Longer Hours
Nurses are known for working long hours, often three 12-hour shifts per week, while other nurses work five 8-hour shifts per week. Some states restrict nurses from working more hours than usual (for example, not allowing nurses to work more than 12 hours out of every 24), except in the event of an emergency. Other states have laws against healthcare facilities requiring nurses to work overtime unless there’s a declaration of a state of emergency.
Emergency or Disaster?
COVID-19 hasn’t just been an emergency — it’s been an all-hands-on-deck disaster.
When a national disaster was declared due to the coronavirus, all bets were off when it came to regulating work hours for nurses and other healthcare workers. Nurses went where they were needed, and provided patient care to the best of their ability, despite exhaustion. During the pandemic, nurses found themselves working nearly non-stop, sometimes unable to leave the hospital between shifts. Hospital wings were filling up so quickly that beds were unavailable for all the patients needing treatment.
Equipment for treating patients — such as ventilators — was also in scarce supply, leaving doctors and nurses to make difficult decisions about which patients would get the equipment that they needed to survive.
Working extremely long hours is stressful, but working extremely long hours while dealing with life-or-death situations for weeks with no end in sight is exhausting. Nurses have been more than willing to put in the hard work necessary to save as many patients as possible, but doing so takes a toll on each nurse’s mental health, physical health, and even their ability to consistently perform to the best of their ability at work.
Emotional Support for Patients
Nurses are trained to use a caring and delicate bedside manner with patients. That doesn’t mean that they’re able to turn off their own emotions when working with patients who are very sick or near death.
Many nurses have told stories of helping patients video chat with their families — all while the nurse knew that it was likely the last time the patient and their loved ones would be able to connect before COVID took its final toll. Nurses have discussed being the only person able to stay with a COVID patient as they passed away, due to staff precautions and visitor restrictions.
In addition to being at the front lines, sitting with patients as they died, many nurses were also the point of contact for family members. This could mean sharing with anxiety-stricken loved ones that the worst had occurred — and, in many cases, that they wouldn’t be able to celebrate their loved one’s life with a family gathering.
While nurses are well-prepared to work with grief-stricken family members, no one is well-prepared to do so hour after hour, day after day. Healthcare professionals found it hard to keep up with self-care in the midst of the pandemic, especially when they were unable to engage in many of their regular activities (spending time with friends and extended family, going to the gym, going out to eat, etc).
Keeping Up with Ever-Changing Best Practices
Even those who haven’t been at the front lines of the pandemic have found it hard to keep up with best practices when it comes to safety. For nurses, this has been far more difficult.
When a new virus or bacteria strikes, it takes time for researchers to fully understand transmission. This can mean changing guidelines on how to stay safe. For nurses who have been at the front lines with their patients, this has been especially stressful. Nurses weren’t only working to protect themselves — they were also working to provide their patients with the highest standard of care.
Areas of COVID-19 research that have been disputed or changed rapidly over time include:
- effectiveness of masks and other PPE
- effectiveness of quarantine and social distancing
- methods of transmission
- long-term effects
- vaccine safety
- vaccine effectiveness
While nurses work closely with doctors to discuss and carry out patient treatment plans, it’s hard for any healthcare professional to stay on top of ever-changing information on how to best treat the virus when they’re also managing an exponentially growing workload.
Post-COVID Nursing Shortage
Nurse Safety in Uncertain Times
There are many areas of the way nurses are treated that need improvement and nurse safety is a top priority. As mentioned above, many nurses found that they were depending on making their own masks or wearing cloth masks provided by volunteers. These masks likely protected patients from contracting COVID-19 from a nurse who was unknowingly carrying the disease but didn’t do much to protect nurses from contracting the disease from a COVID-positive patient.
The far more effective N-95 masks have been in short supply since the beginning of the pandemic, largely due to people storming construction supply stores and buying out these highly-effective masks that healthcare workers desperately need.
These issues are springing forth a positive change for nurses: healthcare administrators are finally listening as nurses demand protective equipment at work. In the past, shortages of nursing equipment were easily swept under the rug. Today, both healthcare workers and the public are hugely aware of PPE supply issues and are supporting nurses as they stand up for their right to stay safe as they work with patients.
In April 2020, National Nurses United held a protest at the White House, demanding that Congress pass laws to provide nurses with the safety equipment they needed to treat patients during a pandemic. While nurses have always been on the receiving end of appreciation weeks and other halfhearted thank-you attempts, both the public and the government have begun to understand what nurses go through to treat their patients.
Mental Health for Nurses
Many nurses have realized how important it is to prioritize their mental health — both in and out of the workplace. Some nurses have found that it’s more important than ever to find time for a 10-minute walk outside or to sit in a staff room and spend some time on a mediation app before re-engaging with patients. While patient care is always a nurse’s top priority, many nurses (and hospital administrators) have begun to understand the need for nurses to have a work-life balance.
Nurses have shown an incredible ability to adapt despite difficult circumstances. It’s hard to say whether the nursing profession attracts people who can creatively come up with solutions to problems, or whether the nursing profession helps to grow problem-solving skills. Either way, nurses should only have to use their ingenuity from time to time — it’s not good for a nurse’s mental health to constantly have to come up with new ways to do more with less.
Nurses are Giving by Nature
Studies show that more than half of nurses put the safety of their patients above their own. Many nurses are giving by nature and may have a tendency to put themselves on the back burner. It’s vital that nursing programs and healthcare organizations alike prioritize both encouraging and providing nurses with self-care opportunities to allow them to take care of themselves so that they can continue to provide excellent patient care.
That being said, it’s likely that nurses will continue to be looked to for new innovations, creativity, and ways to solve problems that seemingly do not have an answer. Post-COVID nursing education may put an emphasis on how to get creative and develop solutions using only the tools at hand, further developing a nurse’s ability to find in-the-moment answers to difficult challenges.
Education and Training: What Could Change?
Nurse education is demanding, and post-COVID nursing education is not going to change that. The intensity of nursing school ramps up over time, culminating in clinical work. Getting used to a new work environment, working long shifts, and working to put classroom topics into practice can all take a toll on a new nurse. The answer to helping nurses become better prepared for patient care may not be teaching them more information because of COVID — rather, it may be choosing the information that’s absolutely necessary for providing excellent patient care, and leaving out information that doesn’t directly relate to positive patient outcomes.
Nursing educators recognize the importance of emphasizing infection control protocols, including:
- disease transmission
- hand washing
- PPE effectiveness
- surveillence and detection
- quarantine
- social distancing
- isolation
- population health
In addition to emphasizing these topics, nursing educators believe that it may make sense to pare down other aspects of the curriculum. Nursing school is incredibly difficult, and adding a new infectious disease protocol on top of other topics may not be the answer to creating a more effective, efficient group of future nurses.
While new curricula are still being developed for nurses, it’s likely that changes to the NCLEX will occur as a result of changes in nursing due to COVID. Nurse education organizations recognize the importance of preparing nurses for their vital role as core healthcare providers during a pandemic.
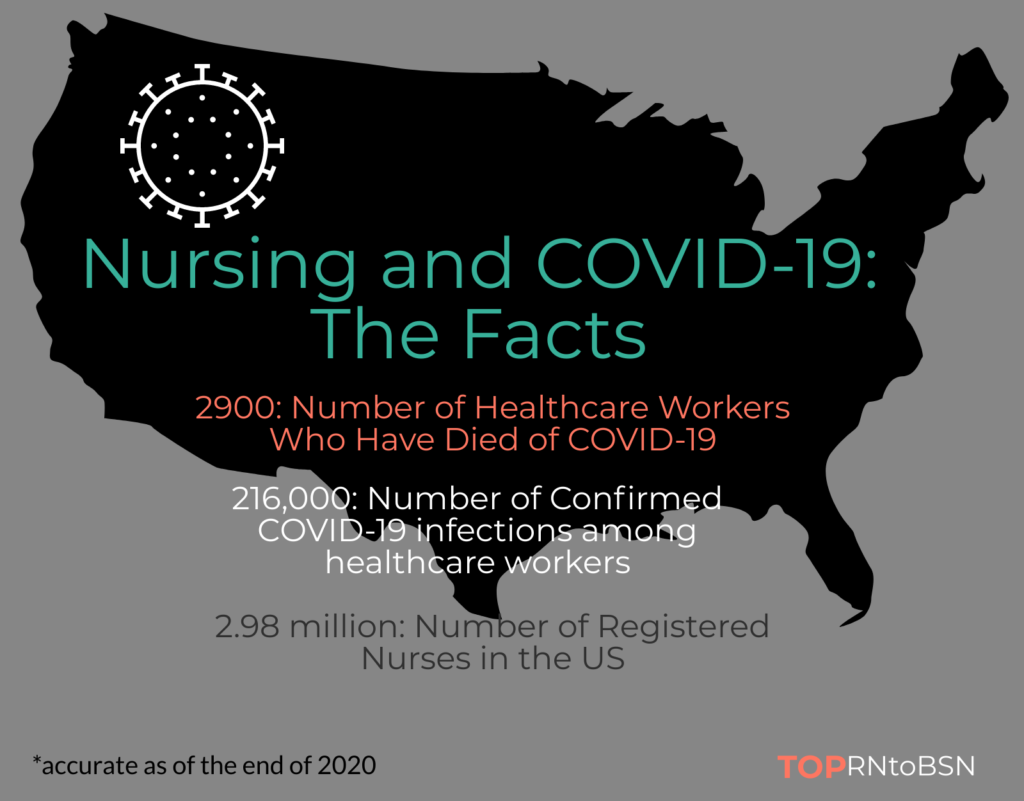
Nurses Lost from COVID-19
Will COVID-19 Happen Again?
One of the most common questions among those who are getting into the nursing field is whether something like COVID-19 could happen again in the future. Researchers say that it’s tough to give a definitive answer at this point.
COVID-19 was an example of animal-to-human viral transmission, and there are other diseases that could take the same route (some with a far higher fatality rate). If nothing else, the COVID crisis has made it clear that healthcare organizations were not prepared for a disaster of these proportions, and major changes need to take place to ensure that if something like COVID happens again, fatalities due to lack of staffing and lack of equipment will be minimized.
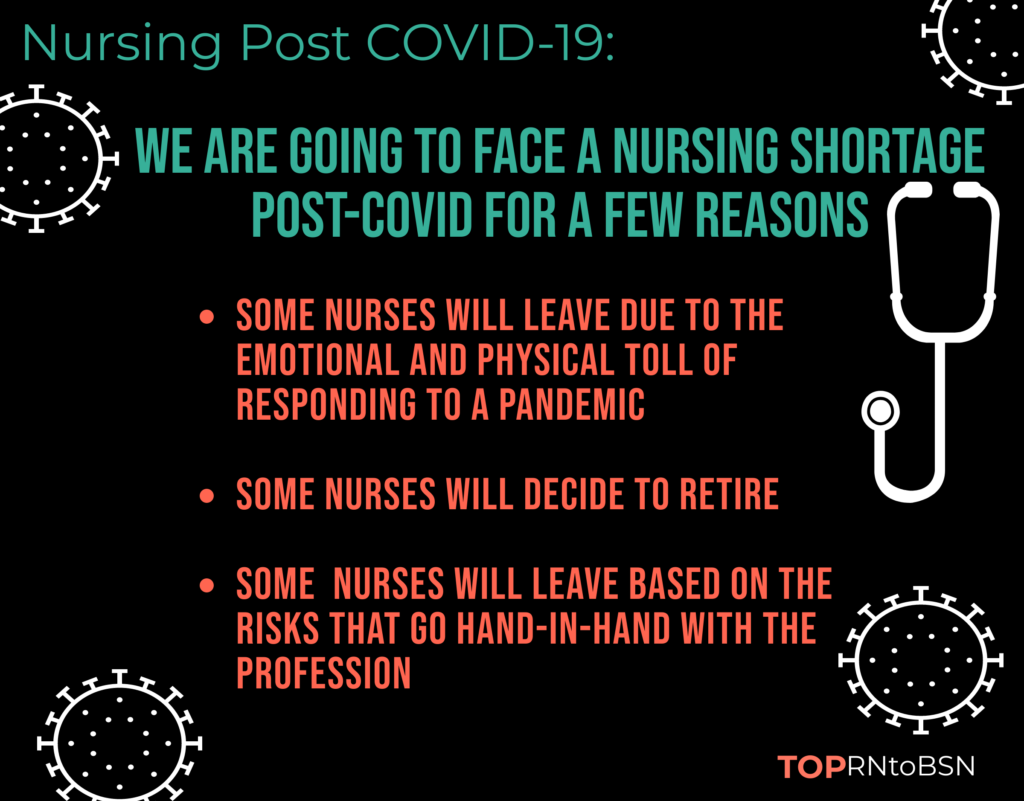
The Nursing Shortage Post COVID
While there has been a shortage of nurses for years, COVID-19 has intensified the problem. As of September 2020, more than 200 registered nurses died due to COVID-19. Many other nurses’ health has been severely affected by the virus, and others still have been forced to change their career trajectory due to family situations related to the virus.
While some nurses have felt more committed to their careers than ever, others have decided that it’s time to pull back, due to stress, an inability to spend time with family, burnout, and more. The need for nurses is staggering — in the next year, over 1.1 million nurses are needed in order to fully staff hospitals and other healthcare organizations.
Due to the COVID crisis, many nurses were suddenly placed in environments in which they had no training. Moving from a direct care nurse for geriatric adults to an acute COVID unit is a huge change, and many nurses are continuing to work in an area outside of their specialty, with no end in sight. A 2020 survey showed that 60% of nurses were considering quitting their jobs, either to move into a new nursing position or into a new career area altogether. Openings for nursing jobs post COVID are likely to be high, with many hospitals and other healthcare organizations needing to fill spots left behind by nurses who have chosen to move on to other fields.
Highest Demand Areas for Nursing Shortage By State
Many of the staffing shortages experienced by hospitals during COVID weren’t only due to a lack of nurses on staff — but also due to a lack of nurses who were able to work. From contacting COVID-19 to quarantine requirements due to a sick family member, many nurses were unable to provide patient care.
It’s vital for healthcare organizations to be aware of how the nursing shortage post-COVID could affect their ability to provide patient care in the event that another pandemic occurs.
Nurses as Administrators and Managers: A Potential Surge
In times of crisis, natural leaders tend to shine, and this is as true in the nursing field as any other. Many nurses have found that they enjoy working as managers, administrators, and leaders within a hospital setting. As well-deserved respect for nurses continues to grow, it’s likely that many nurses will step into managerial roles within healthcare settings.
Some nurses who have focused solely on patient care throughout their careers have found their leadership abilities shining through during the COVID crisis. As more nurses begin to take on leadership roles in hospitals post-COVID, the doors are also opened for current nursing students to think about eventually taking on an administrative position within their future organizations.
Nurses as Advocates: Not Just For Patients, But For Each Other
Nurses have begun to realize the importance of coming together and demanding positive changes in the workplace for their health and safety. This was especially apparent during the PPE crisis experienced by nurses at the beginning of the pandemic.
At the start of the pandemic, many healthcare organizations were keeping nurses from PPE, even though they had the materials necessary to keep employees safe. N-95 masks and other protective equipment were kept under lock and key, supposedly for a time when high-standing healthcare officials deemed it necessary for use. Nurses banded together across the country and demanded better treatment from those in charge.
It’s possible that leadership, advocacy, and team-building may become a part of post-COVID nursing education, as it becomes apparent that nurses must join together in order to get the treatment they deserve from healthcare organizations.
Nursing Post COVID-19
How Telehealth Could Change the Future of Nursing
While some nurses found that they felt fulfilled by providing bedside care to patients during the coronavirus pandemic, others found that they quickly felt burned out, and that bedside care was not the best fit for their career trajectory.
The pandemic has made it clear that telehealth is an effective, convenient way to help people get the healthcare they need, and many nurses have found this to be an enjoyable way of connecting with patients. The future of healthcare will likely provide many nurses with the ongoing ability to treat patients virtually.
Virtual healthcare can make providing healthcare a possibility for a greater demographic of nurses, including those who are unable to work 12-hour shifts, or for those who struggle to stand for long periods of time.
What’s Next For Nursing Students
Like so many things in the world of COVID, it’s hard to know exactly what comes next for nursing students. Much like best practices in nursing, education for nurses and test prep for the NCLEX will continue to evolve. Successful nurses know how to adjust as times changes, implement new best practices, and provide excellent patient care even in the most difficult circumstances. There’s no question that nursing education will adjust to allow new nurses to continue to do so, just as nurses have done for centuries.
Thank you!

Related: