
Nurse Practitioner Prescriptive Authority
Nurse practitioner prescribing laws apply to Advanced Practice Registered Nurses and may vary by state. A Nurse Practitioner (NP) is an Advanced Practice Registered Nurse with responsibilities beyond the standard care offered by an RN.
This individual medical professional can provide a range of additional services and care options, including but not limited to screenings and referrals, diagnostic and treatment, physical exams, health and wellness counseling, and prescriptions for medications, with some possible restrictions based on the state requirements.
What Does Prescriptive Authority Mean?
Independent prescribing or prescriptive authority for APRNs is a privilege granted by state law or regulation that allows certain Advanced Practice Registered Nurses (APRNs) to prescribe medications. These include controlled substances as authorized by their state Board of Nursing. APRNs are licensed to autonomously diagnose, order and interpret diagnostic tests, and manage patients’ overall care. Prescriptive authority allows APRNs to write prescriptions, order laboratory, and diagnostic tests, and provide a wide range of therapeutic interventions, including pharmacological treatments.
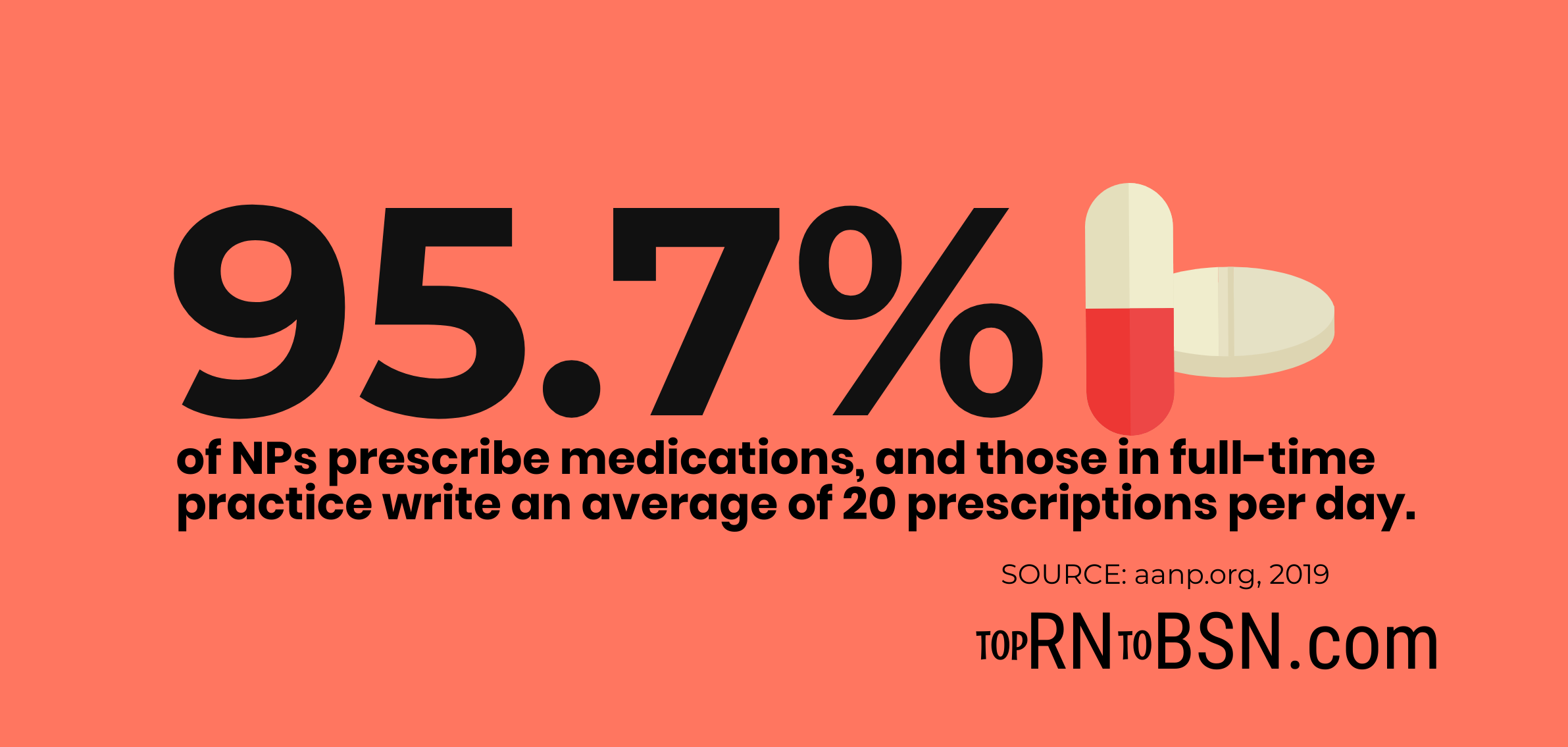
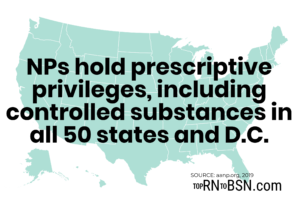
Nurse Practitioner prescriptive authority refers to the ability to write scripts for medication in all 50 states, although the independence with which they can prescribe drugs, medical services, or devices can vary depending on the state laws. The prescriptive authority for NPs is essential for healthcare practice and service. That prescriptive authority provides quality and cost-effective healthcare for patients who need fast, reliable, and accessible care in their communities.
The Nurse Practitioner prescriptive authority has been around since New Mexico first approved it in 2002. Soon after, Louisiana, Illinois, Iowa, and Idaho passed approvals. The American Association for Nurse Practitioners (AANP) recommends that NPs not be restricted. Instead, they encourage NPs to prescribe meds, devices, medical equipment, supplies, and other healthcare services for patients. But, the AANP endorses oversight by the state board and the training, education, and certification credentials.
What are the Additional Educational Requirements for NP Prescriptive Authority?
In order to obtain prescriptive authority, Nurse Practitioners must typically complete additional educational requirements, such as obtaining a Master’s degree and completing an advanced pharmacology course.
Depending on the state, NPs may also need to obtain additional certification or licensure in order to gain prescriptive authority. Additionally, Nurse Practitioners may need to complete a period of supervised practice to demonstrate their competency with prescriptive authority before they are granted full prescriptive authority.
Why is it Important for Nurse Practitioners to Be Able to Prescribe Medication?
NPs who can prescribe drugs fill a crucial role in offering primary care services. They treat populations that may not otherwise have the same access to reliable and cost-effective healthcare or medical services. And this is true, especially in rural and underserved communities and high-population areas. In addition, NPs have advanced training and often have additional specializations and certifications. Many of these skills allow them to also provide comprehensive care options and treatment to the populations they serve.
The prescribing privileges for Nurse Practitioners include a range of responsibilities for diagnostics, interpretation of results, counseling, exams, etc. In addition, a Nurse Practitioner can pursue several additional specialties and certifications in Women’s Health, Neurology, and Cardiology. However, there are other concentrations that are available in Nursing and specifically for Nurse Practitioners.
A Nurse Practitioner prescribing authority is a significant development. According to the American Association of Nurse Practitioners (AANP), NPs step up to provide services in growing numbers. The idea of nurse training to a level where they would offer primary care services has been around since 1965 when Dr. Henry Silver and Loretta Fox joined forces to develop a certification program. In the intervening decades, the program has evolved and grown.
More than 245,000 NPs are now licensed to practice in states across the US. Each of the NPs sees an average of 24 patients every day, which takes on an enormous amount of healthcare coverage. It helps to address the massive demand for primary care that was already evident in 1965. The job growth outlook is at 46%, higher than the average for career opportunities in the US.
What is Scope of Practice?
A Nurse Practitioner’s prescriptive authority is regulated by the state boards of Nursing. The prescribing authority is licensed and regulated to promote public safety. But the question is: Can an APRN prescribe medications? The APRNs can prescribe medicine based on the authority granted to them by their licensing state and the state board of Nursing. For each state and particular individual’s situation to keep up-to-date on the current status of prescriptive authority and licensure.
| Scope of Practice | Description |
|---|---|
| Restricted Practice Authority | Practicing Under Physician Supervision |
| Reduced Practice Authority | Practicing in Collaboration with a Physician |
| Full Practice Authority | Practicing Independently |
A Nurse Practitioner prescribes drugs, including a controlled substance, with and without the collaborative support of a physician. With the growth of job opportunities for Nurse Practitioners, the role has taken on ever-greater responsibilities. It includes providing high-quality care and prescriptive authority. The job of NPs is essential since they are fully authorized to offer healthcare services in rural and underserved areas. These areas would not otherwise have the level of community medicine or prescriptive medical services available.
Why Do NPs Prescribe Drugs?
Even in urban areas, a Nurse Practitioner can help cover a range of services with prescriptive authority. But, they also assist with a wide range of other diagnostic care, testing, and also treatment options for clinics and community medical centers. Part of the reason NPs fill this role is that their salaries are often lower than those of medical doctors.
So, it may be more likely that the non-profit organization or otherwise budgetary-challenged small community can afford to hire them. As a result, NPs are meeting the needs of patients in evolving non-traditional settings. Furthermore, these settings are all over the US to address the shortage of physicians and a growing aging population. In these places, NPs can diagnose and treat patients without physician oversight.
Beyond the obvious reasons for NP involvement in the care and treatment of patients, there’s a difference in how NP treat their patients. In general, they pursue a more holistic approach for the patients they serve. This approach can take on a more consultative or counseling-focused focus. It’s more in keeping with the often more integrated approach that the Nursing profession has with the care and treatment of a patient. It can also involve discussions and counseling on lifestyle choices and other factors that affect the patient’s overall health and wellness.
Are There Limits to the Nurse Practitioner Prescribing Laws?
What medications can Nurse Practitioners prescribe? Nurse Practitioners can prescribe medications with varying layers of physician oversight. Some states support reduced, restricted, and full-practice authority. As a result, NPs can prescribe antibiotics, birth control, and other non-controlled substances in all 50 states.
What Drugs Can a Nurse Practitioner Prescribe?
As a highly educated and experienced medical professional, a Nurse Practitioner can prescribe antidepressants like Prozac and Zoloft. Under Alaska Nursing Statutes, NPs must apply to prescribe a controlled substance (Schedule III-V). The Indiana Nurse Practice Act restricts prescriptive authority. It requires an agreement collaborating with a physician and a Controlled Substances Registration (CSR). In addition, NPs can prescribe narcotics in some states without collaboration or a doctor’s oversight. The DEA Definition of Controlled Substance Schedules outlines the categories of controlled substances.
Schedule II Controlled Substances
These drugs have a high potential for abuse and addiction, such as certain opioids, amphetamines, and barbiturates. Prescriptive authority for these drugs is restricted to medical doctors and certain other licensed healthcare practitioners, such as nurse practitioners, physician assistants, and psychiatrists. These practitioners must have a valid DEA registration number to prescribe Controlled Substances.
Schedule III Controlled Substances
Medications in Schedule III have a moderate potential for physical and psychological dependence. They have a lower risk of abuse than Schedule II Controlled Substances but a higher risk of abuse than IV. Examples of a controlled substance in Schedule III include certain anabolic steroids, certain barbiturates, and certain stimulants.
Schedule IV Controlled Substances
These substances have a low potential for abuse, with mild or low physical dependence or psychological dependence. Examples include alprazolam (Xanax), clonazepam (Klonopin), diazepam (Valium), lorazepam (Ativan), and zolpidem (Ambien).
Schedule V Controlled Substances
The least restricted class of controlled substances is V. This class includes substances with a low potential for abuse, such as cough suppressants, anti-diarrheal medications, and anti-anxiety medications. An example is cough suppressants containing codeine.
Do NPs Have the Authority to Prescribe Schedule II Controlled Substances?
The care of a Nurse Practitioner is comparable to that of a doctor. Therefore, maintenance and prescribing authority are essential. However, nurse involvement does replace doctors but instead works collaboratively together. The Nurse Practitioner’s controlled substance prescribing medications must include the DEA registration number. For Schedule II drugs, the Nurse Practitioner’s authority is the most restricted. For example, NPs can only write scripts for a 30 day supply in North Carolina, Pennsylvania, and Illinois. And in Alabama, NPs can prescribe with a special permit approved by the Alabama Board of Medical Examiners (ALBME).
With the ongoing opioid crisis, the focus on prescriptive authority and ethical ramifications has taken center stage. NPs may be in the best position to advocate for their patients. They are ideal because they have a complete understanding and evaluation of the current and needed pain management, particularly with a background in Pharmacology. Ongoing education and follow-up are always required for NPs to understand their roles as advocates for their patients. NPS offers a level of education directly to their patients that should help mitigate oversight and misinformed prescriptive authority.
Nurse Practitioner State Practice Environment
The Nurse Practitioner practice regulations and restrictions on prescriptive authority are controversial. While the American Association for Nurse Practitioners (AANP) points to the years of safe, reliable, and cost-effective service NPs have offered to their patients, some states do not allow full-practice authority. So, NPs must rely on physicians to fully support their patients’ prescriptive needs.
So what are the States that allow an NP to Prescribe Independently? The Nurse Practitioner prescribing laws by state vary based on collaborative practice, full authority, or required supervision.
Restricted Practice States
The Nurse Practitioner’s prescriptive authority by state requiring supervision and a collaboratively written prescription includes California, Florida, Georgia, Michigan, Missouri, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, and Virginia.
Reduced Practice States
In reduced practice authority states, nurse practitioners can perform some of their scope of practice without physician supervision. State law requires a career-long regulated collaborative agreement with another health provider for the NP to provide patient care, or it limits one or more elements of NP practice. In many states, the nurse practitioner’s prescriptive authority includes a collaborative or reduced approach.
These states include Alabama, Arkansas, Illinois, Indiana, Kentucky, Louisiana, Mississippi, New Jersey, Ohio, Pennsylvania, West Virginia, and Wisconsin. American Samoa, the US Virgin Islands, and Puerto Rico are also reduced practice.
Full Practice States
In full practice authority states, nurse practitioners can perform the full scope of practice without a supervising or collaborating physician. NPs in these states can diagnose patients, prescribe medication, order tests, and operate their own independent practices.
The states with prescribing rights for Nurse Practitioners with full authority with state licensure include Alaska, Arizona, Colorado, Connecticut, Delaware, the District of Columbia (DC), Hawaii, Idaho, Iowa, Kansas, Maine, Maryland, Massachusetts, Minnesota, Montana, Nebraska, New York, Nevada, New Hampshire, New Mexico, North Dakota, Oregon, South Dakota, Rhode Island, Utah, Vermont, Washington, and also Wyoming. The territories of the Northern Mariana Islands and Guam are also full practice.
Evolving State Laws
State restrictions and authorizations for the prescriptive authority of Nurse Practitioners under the law and state boards are in a state of evolution. The prescribed authority of Nurse Practitioners can be somewhat contentious based on the position that some physician groups take on the topic. Still, the trend is moving toward more extraordinary power as NPs continue to fill the gaps in care availability and necessity.
More than 58 million Americans face the side effects of the shortage of inadequate physician availability in their communities. In addition, with their growing importance in health and medical care, nearly 50% of NPs now have hospital privileges that allow them to order specialty services as part of the quality of care.
Related:
- Best Nursing Careers Based on Salary and Demand
- Highest-Paying Travel Nursing Positions
- Unusual Nursing Certifications
- 15 Best Online RN to BSN Programs in MA
- Understanding Ethical Practice
- Therapeutic Communication
- Techniques of Physical Assessment
- Fluid and Electrolyte Imbalances
- Medication Administration
- 10 Highest Demand Areas for Nursing Shortage By State






